If you've ever watched a loved one battle cancer—or been on that journey yourself—you already know the harsh truth: the pain is real, the nausea is relentless, the appetite is gone, and the side effects of treatment often feel worse than the disease. So when patients say cannabis helps, it shouldn’t take 10,000 studies for the medical community to take them seriously.
And yet, here we are.
A groundbreaking meta-analysis published in Frontiers in Oncology this month reviewed more than 10,000 peer-reviewed studies covering nearly 40,000 individual data points related to medical cannabis and cancer. The conclusion? Cannabis offers “significant” therapeutic benefits for patients living with cancer—particularly in managing pain, inflammation, appetite loss, and chemotherapy-induced nausea. The research even hints at potential anticancer properties, though that part of the science is still early and evolving.
“Our findings strongly suggest that medical cannabis can significantly improve quality of life for cancer patients,” said Dr. Marcin Chwistek, a palliative care specialist who contributed to the review.
That should be a mic-drop moment. But instead of making headlines, this kind of evidence often gets buried under layers of stigma, regulatory inertia, and pharmaceutical gatekeeping.
What the Study Actually Says (and Why It Matters)
Unlike many smaller or anecdotal reports, this was not a one-off trial or industry-funded white paper. This was the first large-scale systematic review to pull from real-world patient data, clinical trials, lab studies, and pre-clinical research to paint a global picture of how cannabis interacts with cancer care.
Key findings include:
- Robust support for using cannabis to relieve chronic pain in cancer patients, often with fewer side effects than opioids.
- Evidence that cannabis can reduce nausea, vomiting, and anorexia caused by chemotherapy.
- Signals that cannabinoids may have anti-inflammatory and even tumor-suppressing properties—though this area still needs deeper exploration.
- Patients overwhelmingly reported improved quality of life, including better sleep, reduced anxiety, and improved mood.
So why isn’t this the standard of care yet?
A Legal Industry, Still Treated Like a Crime Scene
Here’s where the frustration—and hypocrisy—kicks in. Despite medical cannabis being legal in 38 U.S. states and a growing list of countries worldwide, patients and doctors alike are operating in a legal gray zone.
- Federal law in the U.S. still classifies cannabis as a Schedule I drug—on par with heroin.
- Physicians often lack training or confidence to prescribe cannabis, thanks to outdated curricula and risk-averse healthcare systems.
- Patients have to self-medicate, navigating dispensary menus without guidance while dodging insurance hurdles and social judgment.
If this were any other drug—especially one backed by thousands of studies—there would be a pharma giant running national commercials, lobbyists pushing legislation, and glossy brochures in every hospital waiting room. But cannabis?
Still controversial.
Still marginalized.
It’s Not Just Medical: It’s Political
The Guardian’s recent coverage of this study rightfully noted the disconnect between mounting scientific evidence and glacial policy change. Cannabis remains a politically charged substance, often debated through the lens of moral panic rather than clinical data.
Even in places where medical cannabis is legal, access is uneven. Many cancer patients—especially in rural, lower-income, or conservative regions—struggle to get legal access or face stigma from their care teams. Others simply can’t afford the out-of-pocket costs because cannabis isn’t covered by insurance.
This isn’t just about science anymore—it’s about power, politics, and who gets to control healthcare narratives.
The Blunt Take: Let the Science Lead, Not the Stigma
We’ve reached the tipping point. The science says cannabis helps. The patients say cannabis helps. So what are we waiting for?
If we’re serious about evidence-based medicine, it’s time to:
- Deschedule cannabis federally and integrate it into mainstream care.
- Mandate cannabis education in medical schools and continuing education programs.
- Fund longitudinal research into cannabis not just as a palliative tool, but as a potential anticancer agent.
- Give patients access, insurance support, and dignity—without treating them like criminals or guinea pigs.
This isn’t a radical idea. It’s a rational one.
Because if 10,000 studies don’t prove the point, maybe it’s time to stop questioning the plant—and start questioning the system.
Want more radically honest cannabis coverage?
Sign up for The Bluntness newsletter—where we break through the noise with smart takes, deep dives, and unfiltered commentary on the future of cannabis, psychedelics, culture, and commerce.






 High-THC Weed Explored - The Bluntness Photo by
High-THC Weed Explored - The Bluntness Photo by  High-THC Weed Explored - The Bluntness Photo by
High-THC Weed Explored - The Bluntness Photo by  High-THC Weed Explored - The Bluntness Photo by Maria Fernanda Pissioli on Unsplash
High-THC Weed Explored - The Bluntness Photo by Maria Fernanda Pissioli on Unsplash 




 Union Square Travel Agency: A Cannabis StoreWill Ellis
Union Square Travel Agency: A Cannabis StoreWill Ellis The Flower Lounge at Union Square Travel AgencyWill Ellis
The Flower Lounge at Union Square Travel AgencyWill Ellis Union Square Travel Agency's New Dispensary Opens on BroadwayWill Ellis
Union Square Travel Agency's New Dispensary Opens on BroadwayWill Ellis Union Square Travel Agency designed by Leong LeongWill Ellis
Union Square Travel Agency designed by Leong LeongWill Ellis Union Square Travel Agency: A Cannabis Store designed by Leong LeongWill Ellis
Union Square Travel Agency: A Cannabis Store designed by Leong LeongWill Ellis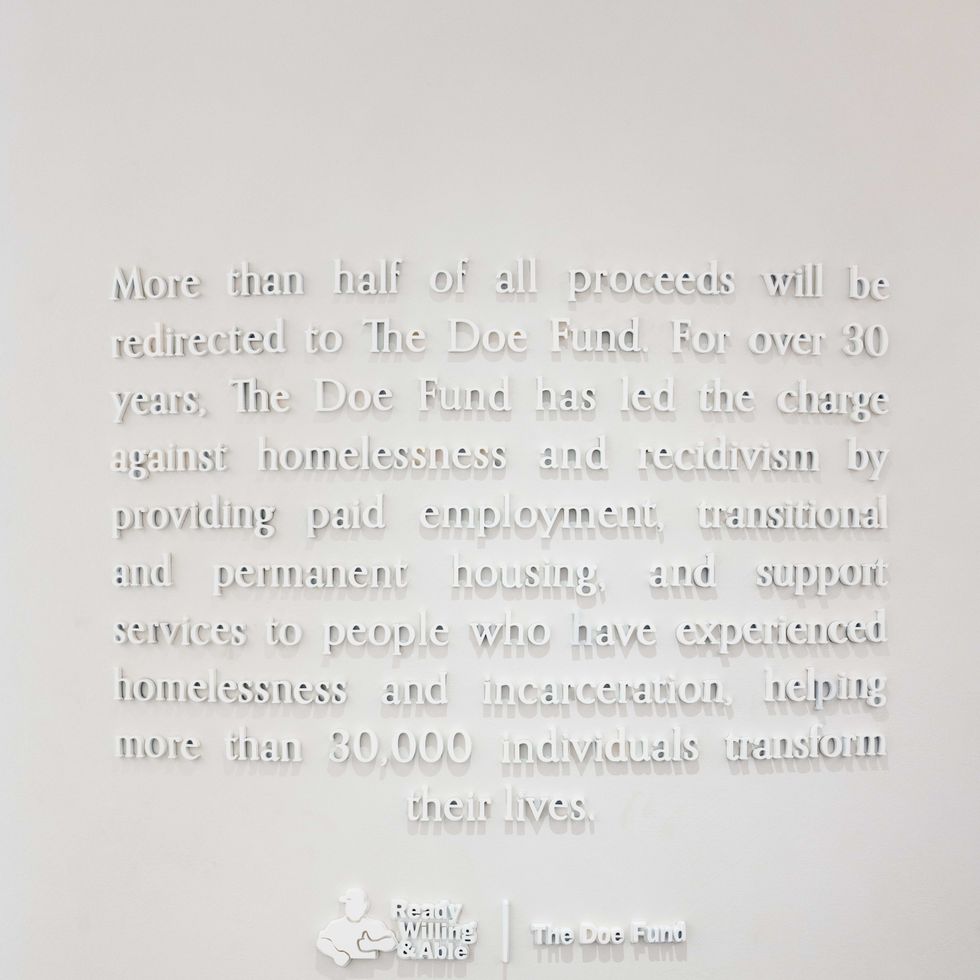 Union Square Travel Agency gives 51% of proceeds to The Doe FundWill Ellis
Union Square Travel Agency gives 51% of proceeds to The Doe FundWill Ellis

 Grateful Dead's Jerry Garcia
Grateful Dead's Jerry Garcia Scene from Reefer Madness
Scene from Reefer Madness  Getting high w/ Awkwafina
Getting high w/ Awkwafina