Forgotten keys, the names of distant relatives, or even the reason you walked into a room — these memory lapses are common experiences. But at what point do these everyday forgetfulness signs indicate something more serious? And what options are available when they do?
When confronting a neurodegenerative condition like Alzheimer’s disease, these questions are just the tip of the iceberg.
Alzheimer’s is a debilitating neurological condition that accounts for a majority of dementia cases. While great strides have been made in our fundamental understanding of Alzheimer’s and its progression, treatment options are still limited, with incredibly few FDA-approved treatments available to the public today.
Several medications do exist to manage the symptoms of Alzheimer’s disease, but this is no easy task, and there is heavy debate on whether the side effects of these treatments are even worth it.
In recent years, evidence has been mounting regarding the potential for psychedelics to enhance neuroplasticity — the brain's ability to form new connections.
Over time, it’s becoming apparent that the intersection of psychedelic research and Alzheimer’s might offer long unanswered questions about the aging brain.
But the question still stands — are psychedelics truly a viable solution for treating Alzheimer’s disease?
The Discovery of Alzheimer’s
In 1901, a physician by the name of Alois Alzheimer came across a patient with an unusual case. The patient, Auguste, had been experiencing eight months of changes to her personality and severe memory impairment.
Auguste frequently found herself lost in familiar situations and fearful of people she knew well. Rife with confusion and fits of jealousy and occasionally imagining that someone wanted to kill her, her husband brought her in to be examined at a psychiatric institution in Frankfurt.
Auguste’s case was of particular interest to Dr. Alzheimer, who had never seen symptoms quite like hers before. He decided to follow her case closely to track her mysterious condition.
In his initial interviews with Auguste, Dr. Alzheimer noted that she would speak clearly and articulate well but would often stop midway through her sentence as if she had become lost.
Over time, her demeanor went from generally anxious, confused, and disoriented to distant, unintelligible, and aggressively reactive. Eventually, Auguste stopped talking altogether and in her final years, became completely apathetic and recluded to her bed.
Perhaps the most tragic and succinct summary of the changes Auguste experienced is from her own remark on her state, “I have, so to say, lost myself.”
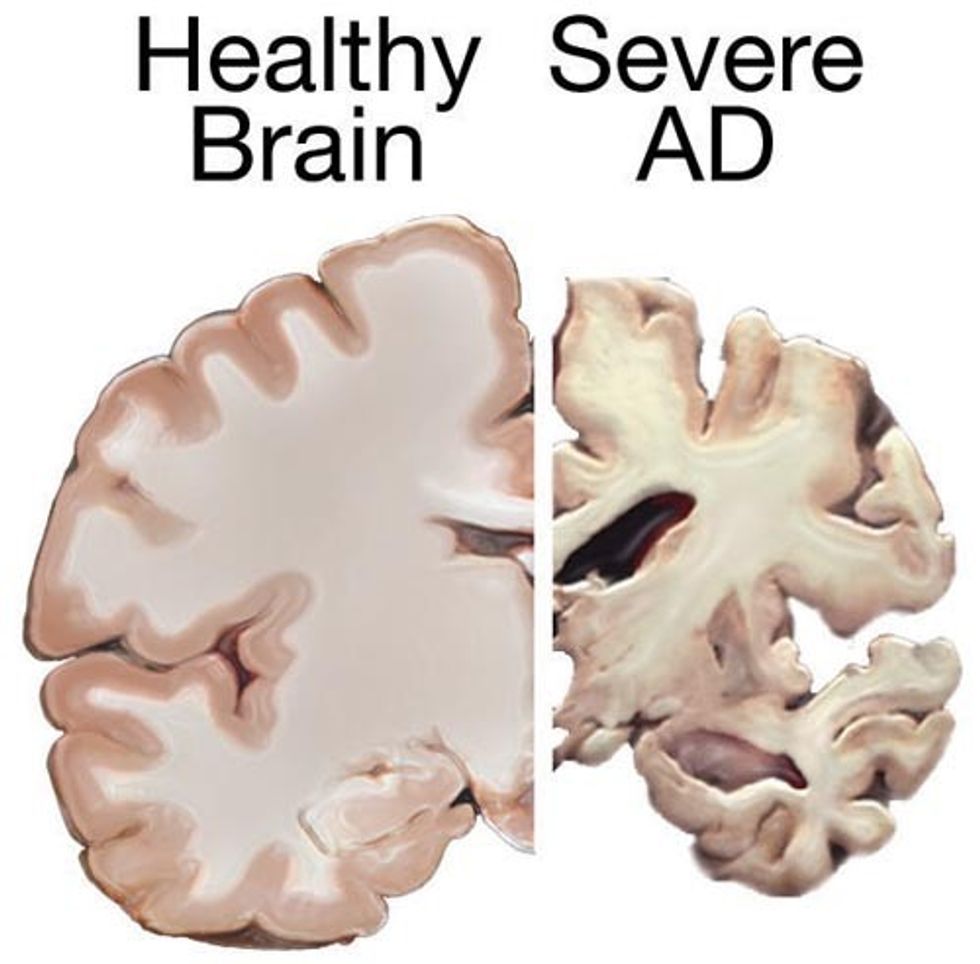
Dr. Alzheimer was not convinced that Auguste's symptoms were psychiatric in nature. When she passed away, Dr. Alzheimer examined sections of her brain under a microscope and found widespread atrophy — a massive loss of cells throughout the brain.
He also discovered thick fibrils called neurofibrillary tangles within the neurons and an unidentified substance, now known as amyloid plaques.
In this discovery, Dr. Alzheimer found what would become known as two of the defining features of Alzheimer’s disease today and set the stage for understanding this neuropathological disease.
What Causes Alzheimer's Disease?
Before we get into the weeds about how researchers believe certain psychedelic substances can be used to counteract the devastating effects of Alzheimer's disease, it's important to understand what, exactly, is happening in the Alzheimer's brain:
Alzheimer’s disease is characterized by two key pathological features:
- A formation of neurofibrillary tangles made up of dysfunctional TAU proteins.
- Plaques consisting of a sticky compound called amyloid-beta that forms around the neurons.
Over time, TAU proteins and amyloid-beta plaques cause damage to the neurons by choking them out and disrupting their ability to function — ultimately leading to widespread neuronal death and inflammation.
As our neurons die, we experience lapses in memory and cognitive decline (confusion, disorientation, mood changes, and difficulty communicating with others).
1. TAU Protein Tangles
TAU proteins are normal components of a healthy brain. They're used to stabilize a group of structures called microtubules that help transport nutrients within the cell.
For reasons not well understood, Alzheimer's disease sufferers have a problem regulating these TAU proteins. They become hyperphosphorylated, which causes them to misfold and form thick tangles that not only don't function as intended but also actively disrupt the neuron's ability to transport nutrients.
This eventually causes the neuron to die.
2. Amyloid-Beta Plaques
Amyloid-beta is another completely normal byproduct of healthy neurons. It forms when another compound called amyloid precursor protein (APP) breaks down.
Normally, this protein is cleared from the neurons by the glymphatic system before it can cause any damage. However, patients with Alzheimer's disease are unable to effectively remove this sticky substance. The exact reasons for this remains unknown. As amyloid-beta accumulates in the brain, it begins to form a thick plaque on the outside of neurons, disrupting communication between them and further contributing to neuronal damage and inflammation.
3. Inflammation
Inflammation is a secondary effect of Alzheimer's disease. As TAU proteins and amyloid-beta wreak havoc on the neurons, the dying cells release proinflammatory cytokines that signal widespread inflammation throughout the brain.
This inflammation further worsens neuronal damage and can cause harm to other unaffected regions of the brain.
Chronic (long-term) neuroinflammation has been linked to difficulty sleeping, anxiety, and depression — just to name a few.
Pitfalls in Current Alzheimer’s Disease Therapy
There are currently only two FDA-approved treatments for Alzheimer’s that target the underlying mechanisms of the disease.
The medications, aducanumab, and lecanemab, were only approved in 2021 and 2023, respectively, and are designed to target and reduce the presence of amyloid-beta plaques.
There's a great deal of controversy around these medications, as it is still uncertain whether the reduction of amyloid plaques can actually translate into meaningful clinical benefits (evidence is mixed on this matter, with some finding marginal improvements and others showing no functional improvement whatsoever).
High costs and the risk of serious side effects such as brain swelling and bleeding further add to the debate about whether the benefits of these medications outweigh the risks.
Ultimately, the efficacy of these treatments remains questionable, leaving a significant gap in effective Alzheimer’s therapies.

Can Psychedelics Slow the Progression of Alzheimer’s Disease?
There are thousands of known chemicals, natural or synthetic, that could be considered “psychedelic.”
Only a tiny fraction of these compounds have been explored as a potential treatment for brain disorders like Alzheimer's Disease.
For the purposes of this discussion, we're specifically talking about "classical psychedelics" — which include tryptamines like LSD (lysergic acid diethylamide) (lysergic acid diethylamide), magic mushrooms (psilocin & psilocybin), and DMT (dimethyltryptamine), and certain phenethylamines like mescaline or DOI.
These psychedelics all work through a similar mechanism of action — they mimic the neurotransmitter serotonin.
There are 15 different types of serotonin receptors in the brain — each one involved with regulating different processes. Psychedelics can bind to various serotonin receptors but are especially active on a particular subtype called 5-HT2A. The activation of this serotonin receptor subtype is critical for the psychedelic experience to take place.
What makes this receptor even more interesting is its apparent role in regulating neuroplasticity — which is the ability of the neurons to adapt and reorganize — restructuring themselves and forming new connections with neighboring neurons.
The ability to support neuroplasticity is considered the key mechanism for the therapeutic potential of psychedelics in the treatment of neurodegenerative disorders like Alzheimer's disease as well as depression and PTSD.
Before we get into the specifics of how researchers are testing the use of psychedelics for Alzheimer's disease, I have to issue a disclaimer:
As of right now, there is no conclusive evidence that psychedelics can directly treat the disease in the same way that amyloid-targeting drugs like aducanumab or lecanemab do. The research we're going to explore below is mostly theoretical and addresses more of the underlying mechanisms involved with the disease.
With that said, there are some very promising preclinical studies and early-stage research that suggest psychedelics like LSD, psilocybin, and DMT may provide a novel approach to fighting or even preventing the development of Alzheimer's disease.
1. Restoring Connections: Psychedelics & Neuroplasticity
New research suggests psychedelics may help restore the brain’s ability to form new connections — which is crucial for combating the neural deterioration seen in Alzheimer’s disease. Substances that accomplish this are called "psychoplastogens."
Dendrites are spindly, branch-like extensions found on the body of neuron cells. Each dendrite has many tiny protrusions called dendritic spines. These spines allow connections to form between neurons so they can communicate.
The dendritic spines are like connecting roads that allow small side streets to merge into to larger highways. These highways allow the movement of information from one region of the brain to another.
Alzheimer's disease erodes these connecting roads — preventing effective communication between neurons. The result is memory loss and cognitive impairment.
A healthy brain has a vast network of dendrites, each densely packed with tiny connecting spines.
A study from 2021 found that psilocybin (one of the active constituents in magic mushrooms) can increase the formation of these dendritic spines — particularly in the frontal cortex. This part of the brain is responsible for many of the higher-level cognitive functions that are responsible for executive control, such as decision-making and emotional regulation.
The formation of new dendrites is part of a larger phenomenon called “neuroplasticity,” which is probably the biggest buzzword regarding psychedelics today.
There's a lot going on with this process, and neurologists are just now starting to understand the mechanisms behind it.
What we do know is that plasticity is severely impaired in Alzheimer’s disease, and a gradual loss of these connections is a hallmark feature of the disease.
Other classical psychedelics have also shown a similar capacity for enhancing plasticity in the brain:
- LSD — A single dose of LSD was shown to influence the expression of many genes related to plasticity in rat brains. Experiments with human neurons have found similar improvements.
- DMT — In 2018, a group of researchers discovered that DMT increased the density of dendritic spines. This improvement was comparable to ketamine, which is currently serving as the gold standard for psychoplastogen research. The difference was that DMT also brought clear functional improvements where ketamine did not.
- DOI — This phenethylamine-based psychedelic was shown to increase the size of dendritic spines on cortical neurons.
2. Protecting Microglia & Curbing Neuroinflammation
Psychedelics may help reduce harmful brain inflammation by soothing overactive microglial cells — potentially slowing the progression of Alzheimer's disease.
Chronic neuroinflammation is one of the key byproducts of Alzheimer's disease. As the neurons break down and die, they release a cocktail of inflammatory cytokines into the surrounding area.
This sounds the alarm for the brain’s resident immune cells (called microglia), which are forced to work overtime in an attempt to repair neuronal damage.
Unfortunately, the constant activation of these cells leads to issues with desensitization and deficiency. Ultimately enabling an acceleration of neuronal death and further buildup of toxic proteins like amyloid-beta. This, in turn, leads to more neuroinflammation, and the cycle continues.
Psychedelics have been shown in preclinical studies to reduce the overactivation of microglia and the production of inflammatory cytokines. These effects have been noted in ketamine, psilocybin/psilocin, and LSD.
By pressing the brakes on these immune system responses, psychedelics may give the immune system a chance to recover and slow the destructive snowball effect triggered by Alzheimer's disease.
3. Fueling the Brain: Psychedelics & Glucose Transport
Psychedelics may enhance glucose metabolism in the brain, offering a potential boost to energy supply and cognitive function in Alzheimer's patients.
The brain requires a substantial amount of glucose (sugar) to function properly — about 20% of the body’s total energy supply. Without proper glucose regulation, cognitive functions like memory, attention, and decision-making can quickly deteriorate.
Changes in how the brain processes glucose are common in Alzheimer’s disease. Glucose, a simple sugar, is the brain’s main source of energy and is crucial for normal brain function. With Alzheimer’s disease, the brain becomes less effective at using glucose for energy.
One study demonstrated that an acute dose of psilocybin increased glucose metabolism by approximately 25% in areas such as the frontal cortex. Similar findings have been reported for psychedelics such as LSD and mescaline — however, no conclusive findings have yet been published.
What this means is that psychedelics may help improve the brain’s ability to use glucose, potentially supporting brain function and ameliorating cognitive loss in regions affected by the progression of Alzheimer’s disease.
4. Emotional Health: A New Approach to Managing Depression
Psychedelics may offer a breakthrough in managing depression for Alzheimer’s patients, potentially improving emotional health and slowing cognitive decline.
As many as 50% of Alzheimer's patients are also diagnosed with depression. Recent studies also suggest that SSRI medications and talk therapy are less effective in this population than in healthy individuals.
The impact of psychedelics on mood has been one of the most extensively studied effects to date. There are an ample number of studies showing that psychedelics have great potential in treating depression, even in cases resistant to traditional treatments.
Research has shown that psychedelics can foster profound emotional experiences and enhance feelings of connectedness, which may help alleviate feelings of isolation and despair often experienced by Alzheimer’s patients.
Several psychedelics have individually demonstrated an ability to alleviate depression symptoms:
- Ayahuasca — A shamanic Amazonian brew containing DMT and various harmala alkaloids has shown clear antidepressant benefits lasting up to 21 days without follow-up treatment.
- DMT — Isolated N,N,DMT has shown similar neurological changes as found in ayahuasca (increases in connectivity and neuroplasticity, for example); however, we have yet to see any actual clinical trials to confirm these findings. Antidepressant effects have also been reported for 5-MeO-DMT.
- Psilocybin/Psilocin — One clinical trial found that after two sessions, 71% of patients experienced a reduction in depression scores by more than 50%. Other studies have noted results ranging from 80% to 100% remission rates in the weeks following treatment with psilocybin.
- Ketamine — Demonstrated rapid (but temporary) antidepressant action after just one treatment. This is probably the most researched psychedelic for the purpose of treating depression.
- LSD — A phase II clinical trial funded by MindMed concluded that LSD had "significant, rapid, durable, and beneficial" effects on major depressive disorder compared to the control group.
The Road Ahead: Psychedelics in Alzheimer’s Research
Over a century has passed since Alzheimer’s Disease was first identified. Yet, with everything we know so far about the underpinnings of the disease and the promising potential for psychedelics to support patients diagnosed with the disorder, we've made very little progress over the last 10 years.
So why has research been so slow?
At the moment, the main obstacle to progress is the fact that most psychedelics are classified as Schedule I drugs. The definition of this category assumes these drugs have no medical value — so gaining access to investigate their medicinal potential is mired in red tape.
On top of this, there are complexities inherent to Alzheimer’s disease research itself — such as the need to study brain tissue postmortem and the fact that this disease progresses slowly over decades.
All forms of Alzheimer's disease research are inherently slow and expensive.
Despite these challenges, the potential advantages of introducing psychedelics to Alzheimer’s research far outweigh the risks, and their introduction into this field may offer some of the missing puzzle pieces the field has been searching for.
In fact, the first clinical studies examining the effects of psychedelics on Alzheimer’s are already underway, which will be pivotal in determining how research in this field will develop.
As research advances, we may uncover novel approaches that not only improve cognitive function and emotional well-being for those affected by Alzheimer’s but also enrich the broader field of neurodegenerative disease treatment.
The intersection of psychedelics and Alzheimer’s research holds significant promise, offering hope for new avenues of care for patients and their families.
This article originally appeared in Tripsitter. If you found this post valuable, consider getting a paid subscription to Tripsitter. Your support makes this work possible.










 Introduction to Psychoactive Mushrooms: The Aztec God Strain - The Bluntness
Photo by
Introduction to Psychoactive Mushrooms: The Aztec God Strain - The Bluntness
Photo by  Introduction to Psychoactive Mushrooms: The Aztec God Strain - The Bluntness
Photo by
Introduction to Psychoactive Mushrooms: The Aztec God Strain - The Bluntness
Photo by 
 How to Store Magic Mushrooms
How to Store Magic Mushrooms How to Store Magic Mushrooms
How to Store Magic Mushrooms How to Store Magic Mushrooms
How to Store Magic Mushrooms How to Store Magic Mushrooms
How to Store Magic Mushrooms How to Store Magic Mushrooms
How to Store Magic Mushrooms